Practical Nursing Program
Follow Your Passion and Become a Nurse
Request Information
Practical Nursing
PRACTICAL NURSING
The Practical Nursing Program at Sumner College can fast-track you to a new career as an LPN in just 13 months. If you are compassionate about others and want to make a difference in the field of healthcare, Sumner College may be the right choice for you.
What sets us apart? Let’s start with small class sizes, exceptional clinical opportunities, and employer partnerships that hire over 72% of our students at facilities where they complete their capstone clinical experience. Quarterly Career Fairs and our own Sumner College Medical Club allow students the opportunity to network with employers while attending school.
According to the Oregon State Board of Nursing, 47% of graduates sat for the NCLEX- PN in the state of Oregon in 2022 were Sumner College graduates.
We also provide every student in the program with a Lenovo laptop computer and the support services that foster student success. With a 97% retention rate for the current reporting year, we know what it takes to help that Dream of becoming a nurse a reality for our students.
Ready to take the next step? Download an Information Packet and contact us to set up a tour today!
Classes start every 10 weeks.
WHAT SETS US APART?
- New Term Every 10 Weeks
- 13 Month Program
- 97% Program Retention
- Over 100 Clinical Sites
- 24 Students: Average Class Size
Our Program
PRACTICAL NURSING
Sumner College is committed to providing a strong foundation for our students who are committed to excellence and prepared to begin their journey in a career that provides professional growth and advancement opportunities, while truly making a difference in people’s lives.
Our program embraces the mission of delivering high quality instruction in classroom, skills lab, and clinical settings that ensure students are equipped with the knowledge needed to contribute to the profession and the health care needs of the community.
This program allows students the opportunity to enter into a nursing program without completing prerequisite courses, and term schedules are set up by the college to assure students who complete all of the required courses can graduate in just over a year.
The Practical Nursing Program at Sumner College is approved by the Oregon State Board of Nursing (OSBN) and the Department of Education. We are authorized by the Office of Degree Authorization (ODA) to award diplomas and degrees, and accredited by the Accrediting Bureau of Health Education Schools (ABHES).
If your Dream includes advancing your practice in the future, we’ve got options for you to consider.
Dream It. Do It. At Sumner College.
PROGRAM INFORMATION
- Application Fee: $50
- Registration Fee: $100
- Lab and Technology Fee: $2,600
- Program Tuition: $30,578
Total Cost of Program: $33,328
Book an Accuplacer Exam:
Career Outlook
NURSING CAREER
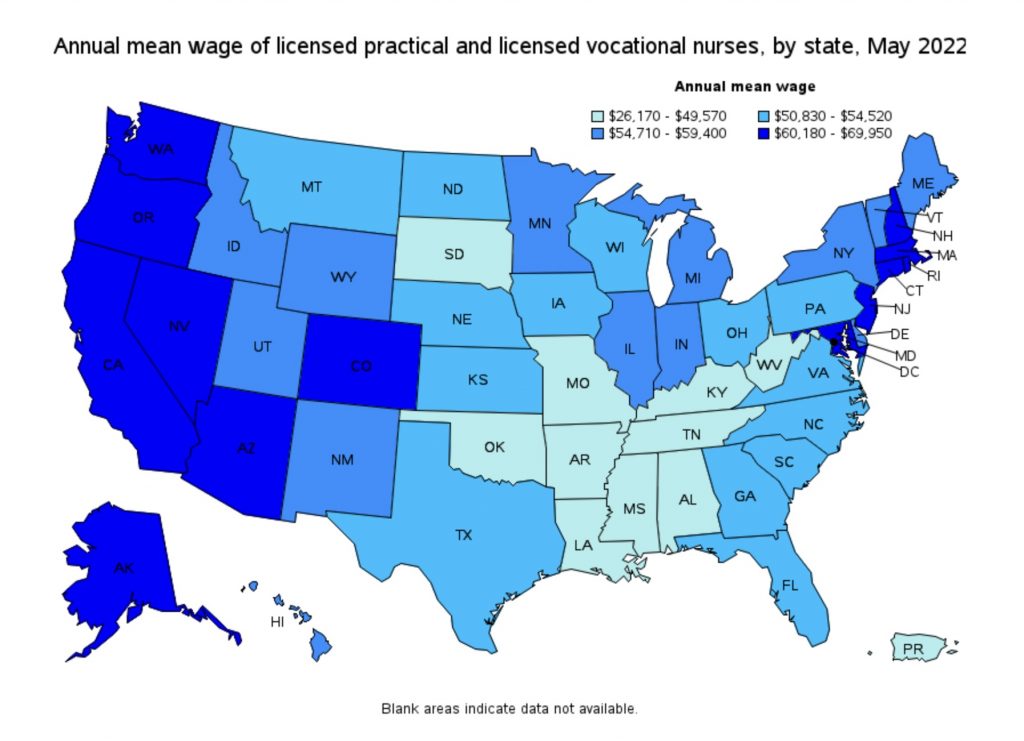
The field of nursing is an occupation that has continued to grow on an annual basis. According to the Bureau of Labor Statistics, employment of licensed practical nurses is projected to grow 11 percent from 2018-2028, much faster than average for all occupations. As the baby-boomer population ages, the overall need for healthcare services is expected to rise. That age demographic, as well as many procedures that used to require a hospital visit now being done outside of hospitals, creates a demand in other settings such as outpatient care centers.
The average median starting salary of our own graduates during the 2023-2024 reporting year was $34.00 per hour.
Where Grads Work
- US Dept of Veteran’s Affairs
- Sono Bello
- Prestige Care
- Avamere
- Vibra Specialty Hospital
- Fresenius Medical Care
- Marquis Companies
- Naphcare
- Action Healthcare
- Clackamas County Corrections
- Columbia River Mental Health
- Fort Vancouver Acute Care
- Frontier Rehab & Extended Care
- The Children’s Clinic
- Vancouver Clinic
- Beacon Bill Rehabilitation
- Columbia Asthma & Allergy
- Hampton and Ashley Inn
- Brookdale Senior Living
- Regency Gresham
- Mirabella
- Washougal School District
- Cascade Park Care Center
- Trilogy Home Center
To find out more about our program, download the Program in Nursing Information kit below and reserve a seat to attend an upcoming Information Session.
13 Months to A New Career
Learn more:
Why Sumner College
- No prerequisites required to apply
- Program designed to be completed in 13 months
- Small lab classes provide individual attention and support
- Graduates are prepared to sit for the NCLEX-PN exam
- Program starts new cohorts every 10 weeks
- Financial Aid for those who qualify
- Hands-on program promotes strong critical thinking skills
- Offering career-focused education since 1974
- 97% Program Retention -2021-2022 reporting statistics annualized
- Over 100 Clinical Sites offer a broad range of learning experiences
- College grants awarded based on academics and attendance
- Career Services Department assists in career placement after graduation

Traci F.
LPN | Charge Nurse & Preceptor
“...if somebody wants to make a career change but is hesitant, I would encourage them to GO FOR IT!”
Read Full Spotlight










LPN V.S. BSN at Sumner College
Understanding the Difference Between LPN, RN, and BSN — and How Sumner College Can Help You Get There When considering a career in nursing, it's…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
WHY EARNING A BSN IS WORTH IT
Why Earning a Bachelor of Science in Nursing (BSN) Is Worth It—Especially at Sumner College Nursing has always been a calling, but today it’s also a…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
A BSN From Sumner College
Begin Your Nursing Career with a BSN from Sumner College in Oregon If you're looking to start a meaningful and rewarding career in nursing,…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
Meet Teresa: Sumner College Graduate
Associate Degree in Nursing Teresa, congratulations on your graduation! As you’ve embarked on your nursing journey, remember: ‘Nursing is not just a profession, it’s a…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
Meet Ana: Sumner College Graduate
Congratulations, Ana! Your hard work, heart, and perseverance have brought you to this incredible milestone. As you begin your journey in nursing, remember: “Nursing is…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
Meet Misty: Sumner College Graduate
Associate Degree in Nursing Misty, congratulations on your graduation! As you’ve embarked on your nursing journey, remember: ‘Nursing is not just a profession, it’s a…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
AI in Nursing: A Trial
AI Note-Taking Tool Gives Nurses More Time for Patients at East Lancashire Hospitals In a forward-thinking move to streamline healthcare and reduce administrative burdens, East…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
Bend Health Fair
Thank you to all who stopped by to say hi at the Bend Health Fair! What a great weekend! Have additional questions? Send us a…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
New Start, May 12!
Congratulations to our newest BSN cohort starting class on Monday in both Portland and Bend! Your new adventure awaits at Sumner College, Dream it Do…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
How Learning Style Impacts You
Welcome to “Understanding Your Learning Style” Unlock Your Academic Potential by Discovering How You Learn Best Have you ever wondered why some study methods work…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
RN Wages
A recent survey conducted by Incredible Health found that registered nurses (RNs) in Oregon earn an average annual salary of $98,630, or approximately $47.42 per…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
TEAS Exam Time!
The TEAS exam is a vital part of the admissions process and an important step toward your future in nursing. To help you prepare, we’ve…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
This week’s Information Sessions
Head over to one of our campuses for a great info session this week! In these sessions, you’ll learn about the application process, including how…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
Changing the Nursing Narrative
The American Nurses Enterprise (ANE- associated with American Nurses Association) has launched a bold new initiative aimed at redefining how society understands and measures the…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
Information Q&A
🌟 Discover Your Calling in Healthcare – Join Our BSN Info Session! 🌟 Sumner Nursing College | Bachelor of Science in Nursing 📅 Classes Begin:…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
Information Sessions
Are you ready to take the next step toward a rewarding career in healthcare? At Sumner College, we are committed to providing you with the…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
Bend, in May!
Take a sneak peek into one of our brand new classrooms at our Bend campus, on campus information sessions are held once a week, register…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
Sumner College Student of The Month | February 2025
Congratulations Josephiene for being the February 2025 Student of the Month at Sumner! CONGRATULATIONS ON YOUR ACCOMPLISHMENT! Meet Josephiene, a dedicated nursing student whose passions…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
TEAS Exam Time!
The TEAS exam is a crucial part of the admissions process and a key step toward your nursing career. To help you prepare, we’ve gathered…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
Nursing in Oregon
Become a Nurse at Sumner College Nursing School in Oregon! Ready to start a rewarding career in healthcare? Sumner College Nursing School offers a…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
International Women’s Day
Thank you to all of the women in our lives, including the majority of our nursing occupations!…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
Apply Today!
Ready to start your nursing career? At Sumner College Nursing School, we offer hands-on training, personalized support, and a pathway to success in the healthcare…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
Become a Nurse!
Nursing offers numerous advantages, making it a rewarding career choice. The profession boasts excellent job security, with a projected 6% growth rate among registered nurses…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
First Day!
Happy first day to our latest BSN cohort, and welcome to the Bend campus!…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
Is Nursing School for Me?
Nursing school is not just an opportunity to build a rewarding career; it’s a chance to make a real difference in people's lives every day.…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
Bend Countdown!
Welcome to Bend! We are excited for our first Bend BSN Cohort to start! Feel free to contact us with any questions!…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
Studying for the TEAS Exam
As part of the admissions process, the TEAS exam is an important step toward your future in nursing. We've compiled a list of helpful resources,…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
What Kind of Nurse Should I Be?
There are many different kinds of nurses, some you may not know had a specialty, including: Case Management, Neuroscience, Telephone Triage, and Forensics. Regardless of…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
17 Days until Bend Launches!
With just 17 days until our first class of BSN's start in Bend, be sure to reach out to our admissions representatives to get all…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn
Helpful Hints!
Nursing students often face a variety of challenges, from long study hours to the financial strain of tuition. The coursework and exams can be intense,…
Share at FacebookShare at TwitterShare at PinterestShare at LinkedIn